Healing ITP: My Path to Understanding and Recovery
Posted by Mira on April 30, 2025 in stories
Immune Thrombocytopenia (ITP) is an autoimmune condition that causes your platelet count to drop, sometimes dangerously low. Before I was diagnosed, I had never even heard of it. When I finally was, I realized how wild and unpredictable this disease can be. It throws your life into a swirl—full of ups and downs like a rollercoaster. Because ITP is rare, it can feel isolating. Sometimes it seems like no one really understands what you're going through.
I'm writing my story in case you’ve stumbled across this post looking for answers, encouragement, or simply someone who gets it. Maybe what I’ve learned so far can help you in some way.
(At the time of writing, my ITP isn’t cured—or, as doctors would say, not in remission yet. But I’m still on the journey, still learning, and I hope one day I’ll be able to update this paragraph with good news.)
Contents
When It All Started
August 2024
In August 2024, my family and I returned to the United States after visiting 10 countries across Europe and Asia. We felt healthy and full of energy—after all, we were still young. That’s why we decided to take on such an adventurous trip.
Shortly after we returned, my menstrual period began, but this time it was different. I started passing large blood clots—something I hadn’t experienced before. I’d had smaller clots in the past, but this felt unusual. I assumed the clots would stop, but they didn’t. As the days went on, I began feeling more and more exhausted. Eventually, I decided to see my family doctor.
My doctor prescribed tranexamic acid (TXA) to help stop the bleeding, and it worked. I thought it was just a one-time issue, something that would pass. However, I continued to feel incredibly tired, so I took a few weeks to rest and recover. At the time, I didn’t realize it, but I was severely anemic due to the blood loss. It was only later that I understood the extent of what was happening.
Octorber 2024
My menstrual period became heavy again, and this time, it was unbearable. I could barely leave the house—every hour, my pad would be soaked, and I had to change my clothes because the blood would stain everything. I continued taking the tranexamic acid (TXA), but it took a long time to show any effect. Eventually, the bleeding stopped.
But one morning, I woke up feeling utterly drained. My husband found me barely able to speak and rushed me to urgent care. There, we learned that my hemoglobin had dropped to 8 — dangerously low. They immediately sent me to the ER for an emergency blood transfusion. That was the moment I truly understood the severity of my anemia, which was caused by heavy blood loss.
When I asked the doctor at urgent care what might be causing the bleeding, she just shrugged and suggested it could be perimenopause. Perimenopause — yet another new term I now had to research.
In early October, I had my annual exam and blood test. My doctor briefly mentioned that my platelet count was low—around 20k (normal range is between 150k and 400k)—but didn’t seem overly concerned about it. Unfortunately, I didn’t fully grasp the significance of this at the time, and I didn’t think to ask more questions.
At that point, neither my doctor nor I connected the dots between my low platelet count and the heavy bleeding. My doctor referred me to an obstetrician/gynecologist (OB/GYN) to look into potential issues with my uterus.
He also prescribed ferrous sulfate to help boost my hemoglobin, and asked me to recheck hemoglobin in 2 months.
November 2024
The OB/GYN appointment had a long waitlist, so I wasn’t able to see anyone right away. My visit was scheduled for December, which meant I had to get through another cycle without knowing what was going on.
In November, my menstrual bleeding was once again extremely heavy. I relied on TXA to help manage it, but just like before, it took a long time to work. I felt helpless, stuck in a cycle I couldn’t control, still unaware that something deeper—like my platelet count—might be playing a role.
December 2024
I finally saw the OB/GYN in December. After an ultrasound and a thorough check, the doctor told me there was nothing structurally wrong with my uterus. But she offered several options to control the heavy menstrual bleeding: birth control pills, an IUD, or even a hysterectomy.
I was surprised. These were all interventions I had avoided my whole life—I’d always preferred a more natural approach. The idea of removing an entire organ to stop bleeding felt drastic to me.
Curious and a bit unsettled, I started doing my own research and talked to a few relatives. To my shock, I discovered just how common hysterectomies were. Many women saw it as a routine solution. It felt almost normalized, like cutting out the uterus was just another medical option—no big deal. But to me, it was a big deal.
After taking ferrous sulfate for two months, I went back to my family doctor to check my hemoglobin levels. When the results came in, he told me everything looked good—my hemoglobin was back to normal. He didn’t mention anything about my platelet count, even though hemoglobin and platelets are reported together in the same Complete Blood Count (CBC) panel.
Later, my husband looked over the results and asked, “Why is your platelet count 16k?” I had no idea what that meant, so I called my doctor. He told me the lab had flagged the result as “clumped,” meaning the platelets might have stuck together and given a false reading. He asked me to repeat the test. I also asked him whether the low platelet count was causing my heavy menstrual bleeding, and he adamantly said no.
I went in for another blood draw. Then, at around 3 a.m., I got a call from the clinic’s on-call doctor. She said she had been paged because my new lab result showed my platelet count was 13—alarmingly low. It was low enough to trigger an emergency alert. She warned me to be extremely careful and told me to go to the ER if I experienced any bleeding or bruising.
After hearing the news, I was terrified. I woke up my husband in a panic and told him we needed to go to the ER immediately.
At the ER—for the second time that year—I didn’t stay long. The doctors diagnosed me with Immune Thrombocytopenia (ITP) and prescribed a high dose of dexamethasone for four days before sending me home. At the time, I thought ITP was just a simple condition, something that could be fixed quickly.
What I didn’t realize was that dexamethasone is a powerful steroid meant to shut down the immune system—its purpose was to stop my body from attacking my own platelets. No one explained that clearly to me, and everything felt so new, so overwhelming. I had no idea this was the beginning of a long and uncertain journey.
They told me to follow up with a hematologist in a few days. I left the ER with a prescription in hand, thinking I’d be better in no time. I was wrong.
Surprisingly, while I was on dexamethasone, my period came—and for the first time in months, it was normal. No heavy bleeding, no large clots. It was an eye-opening moment. I realized my family doctor had missed something important: my heavy menstrual bleeding wasn’t just a gynecological issue—it was directly linked to my low platelet count. He hadn’t caught the warning signs. When platelets are low, your blood can’t clot properly, and that explained everything I had been going through.
January 2025
January 2025 was a rollercoaster. I was on high-dose dexamethasone twice, each time for four days. After each round, my platelet count rose to around 70k — which was encouraging — but then it would drop back down to around 20k. It felt like a constant battle, and I was terrified.
My hematologist dismissed my questions about what could be causing this illness, so I started doing my own research. I bought books, including The Immune System Recovery Plan by Susan Blum and Metabolical by Dr. Robert Lustig. I began learning that there are many types of autoimmune diseases — and ITP is just one of them. A common trigger for autoimmune diseases, I discovered, is leaky gut.
From The Immune System Recovery Plan and some YouTube videos, I also learned that vitamin D deficiency is often linked to autoimmune conditions. I asked my hematologist to check my levels — and sure enough, my vitamin D was extremely low at just 13 ng/mL. The doctor prescribed vitamin D3, 50k IU per week for two months. However, that dose was too high for me, and I couldn’t sleep. I switched to a daily dose of vitamin D3 with K2, 5k IU per day.
My hematologist also found that my ANA marker was elevated and suspected that I might have lupus, which could be the underlying cause of my ITP. He referred me to a rheumatologist for confirmation. When I saw the rheumatologist, he confirmed the elevated ANA and diagnosed me with lupus. It was another shock — and a wave of panic. Before this, I had no idea what lupus was. After just a few Google searches, I quickly realized that lupus is another serious autoimmune condition and many people have to live with it for the rest of their lives.
I hit the bottom of my life in january. The fear of these new diagnoses scared me that I could not think of any other things. It was surely the darkest moment of my life. One moment i was healthy and traveling around the world, and the next moment I was bedridden with a life-threatening illness.
February 2025
February 2025 was the hardest month—but also a turning point.
In my search for a cure, I explored Traditional Chinese Medicine (TCM). I visited a TCM doctor who examined my pulse and tongue and told me that my kidney, spleen, and liver were all weak. He prescribed a different combination of herbs each time I saw him. I took the herbs three times a day.
In the second week of February, my platelet count took a nosedive—dropping to the teens and eventually down to just 2. I was sent to the ER and hospitalized for three days. My hematologist advised me to stop taking the herbs immediately and suspected they were contributing to the sharp decline in my platelet count.
While in the hospital, I started taking Doptelet at 20mg per day. My platelet count began to improve. Finally, I had found a medication that could consistently sustain my platelet levels.
Around the same time, I discovered the carnivore diet, backed by numerous testimonials from people with autoimmune conditions. A family member had also successfully reversed health issues with it. Inspired, I decided to give it a try and completely clean up my diet. My ultimate goal is to reverse ITP and lupus and eventually get off medications. Doptelet was just buying me time.
A huge shift that month was also mental. I transitioned from a victim mindset—constantly mourning my lost health—to accepting my illness and letting go of my fear of death. I used to lie in bed afraid I might not wake up if I started bleeding internally and didn’t have the platelets to stop it. But that fear faded. I told myself, If I die, so be it.
That mindset shift, surprisingly, made me braver and bolder. It gave me the courage to try new things. My parents were still fearful, just as I had been before, but I firmly told them: If you want to support me, you can’t look back either. You have to look forward, like I do now.
March 2025
Someone from an ITP Facebook group suggested that I get tested for an H. pylori infection, which is often linked to ITP. I did some research and found that connection confirmed.
The connection between H. pylori and ITP is well-documented in medical literature. Here are some key studies:
- Helicobacter pylori-associated immune thrombocytopenia: Clinical features and pathogenic mechanisms, 2014
- Helicobacter pylori induced Immune Thrombocytopenic Purpura and perspective role of Helicobacter pylori eradication therapy for treating Immune Thrombocytopenic Purpura, 2021
I took a breath test for H. pylori, and it came back positive. The GI doctor immediately prescribed antibiotics to clear the infection, and I took them for 14 days.
During this time, my platelet count dropped to 40k. My hematologist increased my dose of Doptelet to 40mg per day. But my platelets didn’t bounce back to the 80k level they had maintained before the antibiotics.
He suggested IVIG again to quickly boost my platelets. But I refused. I wanted to wait and see what my body would do once the antibiotics were out of my system.
April 2025
The antibiotics were finished by early April, and by the end of the month, I took a stool test that confirmed the H. pylori infection had been cleared.
My platelet count began to improve, and my hematologist reduced my Doptelet dosage to 20 mg per day. At this point, I was eager to see if my platelet count would continue to improve with the lower dose (20 mg).
I also followed up with my rheumatologist. Through a blood test, he confirmed that my lupus was improving, but it was hard to determine whether my immune system was improving on its own or if it was the effect of the HCQ.
May 2025
The platelet has been steadily improving in May. When the Doptelet dosage was reduced to 20mg per day from 20mg/40mg on alternate days, my platelet count tanked quickly from 168k to 96k. My hematologist suggested I increase the dosage to 20mg/40mg on alternate days again, but I refused. I wanted to see if my platelet count would continue to improve with the lower dose (20 mg), and also wanted to compare the number with the numbers before the antibiotics when I was also on 20mg of Doptelet.
I'm glad that I followed my instincts and kept the dosage at 20mg per day. My platelet count has been steadily improving ever since.
My white blood cell count was also improving, from 2.9k to 5.5k, which is a healthy range.
June 2025
I traveled to Japan in June and maintained a strict diet—avoiding eating out, cooking at my Airbnb, and focusing on meat intake—while doing weekly blood draws. I had them done in Japan, outside of my home state. The results were good.
Starting June 11, I stopped taking HCQ. I suspected it was causing side effects such as muscle pain and, most notably, photosensitivity. I’ve heard that stopping HCQ can lead to lupus flare-ups, but I was willing to take the risk. I had no symptoms before the lupus diagnosis, aside from blood markers that resembled lupus. Ironically, after starting HCQ, I began experiencing symptoms—despite curing my H. pylori infection and maintaining a very clean diet.
On June 13, I received great news: my platelet count was 208k, which is the threshold for reducing my Doptelet dosage. I was so happy. My hematologist suggested maintaining the 20mg daily dosage until I have two consecutive platelet counts above 200k.
For the rest of the month, however, my platelet count dipped to 130k, so I’ve continued taking 20mg daily.
July 2025
We flew to Australia in July. I was able to find a local pathology lab to test my Full Blood Count (CBC) as well as ESR (erythrocyte sedimentation rate, a marker of inflammation).
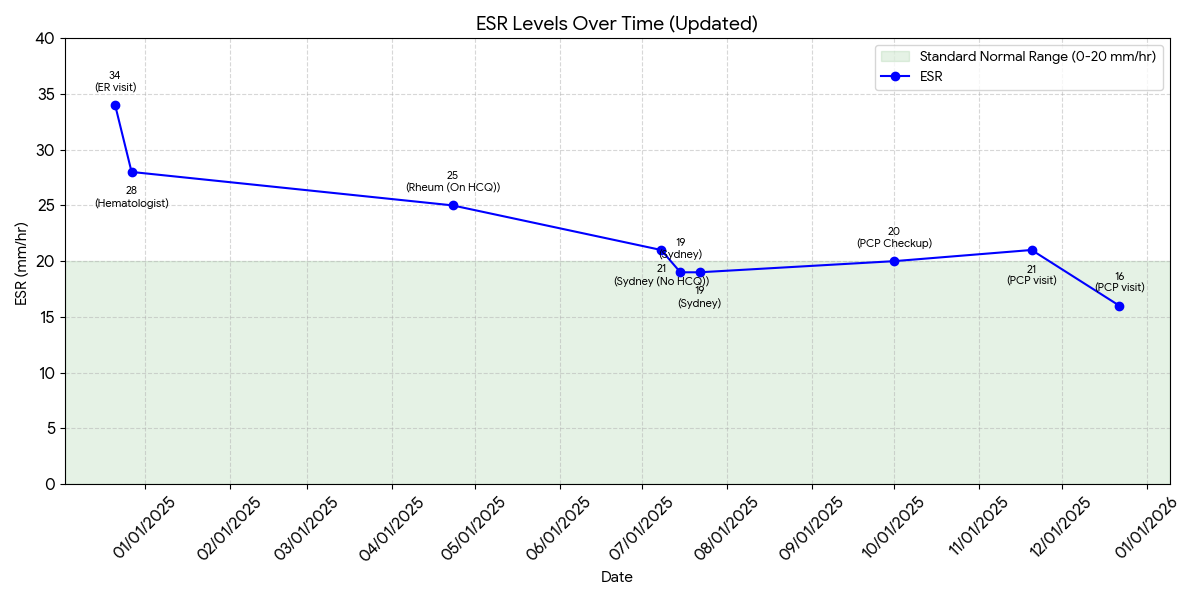
I was surprised to see that my ESR was decreasing—from 25 in April 2025 to 19—even though I stopped taking HCQ in June 2025. It was very encouraging!
I don’t want to jinx it, but honestly, there were many days in July when I didn’t feel any joint pain while walking. It felt so freeing to be pain-free after such a long time.
While in Sydney, my platelet count stayed above 200 in two consecutive tests (see Platelet Counts below), which allowed me to lower my Doptelet dosage from 20 mg daily to just 20 mg three times a week—a huge milestone, and the first time I’ve been able to reduce it this far!
August 2025
We just got back from Australia to the U.S. During the two-month trip, I still had weekly blood draws, which really took a toll on my right arm. Since phlebotomists usually can’t find a good vein on my left arm, they kept using the same vein on my right, leaving it badly bruised. After learning from another ITP patient, I asked my hematologist if we could switch to monthly blood draws whenever my platelet count stays above 100. He agreed.
In August, I only had two blood draws, and my platelet count dropped to 118k—while taking just half of my previous Doptelet dose. I view this as a positive sign. I reduced my dosage from 20 mg three times a week to 20 mg three times every seven days (3/6 → 3/7 of a pill per day), a 14% reduction.
I’ve also had no flare-ups since stopping HCQ, and my photosensitivity is fading. This makes me think the lupus diagnosis may have been wrong. I even canceled my rheumatology appointment to avoid unnecessary blood draws. I’ll still ask my primary doctor in October to check a few autoimmune markers during my annual labs.
September 2025
In September, I continued lowering my Doptelet dosage—from 20 mg three times a week to 20 mg three times every eight days (3/7 → 3/8 of a pill per day). By the end of the month, my platelet count was still around 100k+ (105k). This wasn’t an exciting result, but it shows that my platelets remain stable even with a 12% dose reduction.
This month, I walked outside three times a day: in the morning, after lunch, and in the evening. The Texas sun was still strong in September, and I got tanned—but I still did not get the lupus “butterfly” rash on my face. This again suggests that my lupus diagnosis may have been incorrect.
Another reason I spent time in the sun was to test whether sunlight could help raise my white blood cell (WBC) count. When I was in California, my WBC was very high at 5.5, so I hypothesized that sunlight was a factor. Back in Texas, my WBC dropped to 3.5. After a month of daily sun exposure, my WBC was 3.3—showing no significant improvement. Therefore, my hypothesis was not supported.
October 2025
Since the beginning of October, I have reduced my Doptelet dosage to 20 mg every three days. By the end of the month, my platelet count was still around 100k (99k on 10/22/2025). I consider this a positive sign—stable despite the reduced dosage.
I will continue with the same dosage for now and see if my platelet count continues to improve at next month’s blood draw.
My joint pain is intermittent. There were a few days in October when I did not feel any joint pain while walking. It felt so freeing to be pain-free, something I hadn’t experienced since being in Australia. Then the pain returned, but I still consider this a positive sign. With HCQ, I am having some pain-free days, and overall, it is not getting worse.
November 2025
I have not changed my Doptelet dosage — I’m still taking 20 mg once every 3 days.
In November, my platelet count dropped to 57k on 11/19/2025 and 62k on 11/20/2025, confirmed at my PCP visit. This was a concerning decrease compared to the previous month. The strange thing was that I actually felt great physically, and my menstrual bleeding during that time was the most manageable it had been in months. I’ve been trying to understand possible reasons for the drop:
- I ate a large portion of homemade sourdough bread the day before the test — the first time I’ve eaten that much gluten in a long time.
- One of my kids caught a cold at school. I didn’t have any symptoms myself, but I was exposed to the virus.
I decided to return to my gluten-free diet and planned to monitor my platelet count the following week to see whether it improved.
After 2 weeks, on 12/3/2025, my platelet count recovered to 95k, which is similar to my typical level before the drop. Because of this V-shaped pattern, I suspect the cause was one of the two factors above. I will continue avoiding gluten and focus on keeping myself healthy with a clean diet, at least until I feel ready to test gluten again.
This drop and recovery also made me wonder: is it really necessary to keep my platelet count around 100k with Doptelet? My menstrual bleeding was very manageable even when my platelets were as low as 57k. Would it make sense to lower the dosage further? I’ve also seen people in online communities mention that TPO-RAs may make the bone marrow work too hard, and I don’t want that to happen.
Toward the end of the month, my joint pain started to diminish — sometimes I didn’t feel anything at all. It was also less sunny during that time. It’s hard to tell whether my condition is actually improving or if the change is simply due to the weather.
December 2025
I reduced my Doptelet dosage to 40 mg every seven days, so I expected my platelet count to drop slightly. However, it fell to 74k—a more significant drop than anticipated. Since I was also fighting a virus, I suspect this 20k drop resulted from the combination of illness and the medication reduction.
My menstrual cycle has been manageable this month, which is a good sign. I will continue to monitor it, and as long as it remains stable, I don't plan to have another CBC test until March 2026.
January 2026
I decided to do less testing in 2026. In January, I did not have any blood draws but monitored my menstrual bleeding. It was manageable this month, which indicates that my platelet count likely remained within a safe range. I did not see any blood clots in my underwear, which is very reassuring.
Given this, I decided to further reduce my Doptelet dosage to 20 mg every 4 days (from 40 mg every 7 days). This is a very small dose reduction. I will monitor my next cycle to see how it goes.
Diagnosis
On December 27, 2024, I sat in the hematologist’s office for my follow-up. My platelet count had risen to 78k— an encouraging sign that the high-dose dexamethasone had worked, at least temporarily.
I had hoped to explain how I ended up here: the travel, the exhaustion, the unexplained bleeding, the emergency room visits. But before I could say much, the hematologist handed me a single sheet of paper—my treatment plan. He didn’t seem interested in my story. He was focused only on the protocol.
The paper listed a step-by-step protocol: first-line treatment, second-line treatment, and if neither worked, the final option—splenectomy. Removal of the spleen.
I was stunned. Up until that moment, I still believed ITP was a minor, manageable issue. Now, I was reading about the possibility of permanently losing an organ. The gravity of it all hit me at once. This wasn’t going to be a quick fix. This was going to be a long road.
Treatment Journey
The healing journey has been long and often frustrating. While doctors focused on managing my condition with medications—possibly for the rest of my life—I couldn’t accept that as the only answer. I never stopped searching for the root cause of my illness. I don’t believe this happened because of bad luck or genetics alone. Something triggered it, and I was determined to find out what.
Vitamin D Deficiency
Starting in the new year, 2025, I began reading everything I could about ITP. I learned it was an autoimmune condition, so I dove into podcasts and books about the immune system. One thing kept coming up: Vitamin D deficiency is often linked to autoimmune diseases. I asked my hematologist to test my levels—and sure enough, my Vitamin D was extremely low, just 13 ng/mL.
I started digging into medical papers to see if there was a connection between Vitamin D and ITP. And yes, there was. I began supplementing with Vitamin D3 + K2, and within two months, my levels rose to a healthy 74 ng/mL. I noticed improvements in my energy and mood—but my platelets didn’t return to normal. So while Vitamin D deficiency may have played a role, it wasn’t the root cause of my ITP.
First Line Treatment (Dexamethasone and IVIG)
Dexamethasone is a corticosteroid that works by powerfully suppressing the immune system. It can rapidly boost platelet counts, which is why my hematologist prescribed it—four days at a time, at a high dose, twice. Both times, the pattern was the same: my platelet count would jump to 70k or 80k within days, only to crash back down below 20k shortly after.
My hematologist told me that for some patients, dexamethasone can be enough to restore platelet levels to normal. But for me, it didn’t stick. While I was on it, my face puffed up and turned red. When I stopped, I experienced a prickly pain all over my back. It was miserable. Every time, I told myself, I don’t want to take this again.
Alongside dexamethasone, my doctor also gave me IVIG—an infusion of antibodies designed to temporarily boost platelet levels. It’s a very expensive treatment. Honestly, I’m not even sure it worked for me. It always seemed like the dexamethasone did the heavy lifting.
Once, when my platelet count crashed to just 2k, I had to go to the ER for the third time. The doctors gave me another round of high-dose dexamethasone and IVIG together. It was another desperate attempt to bring my platelets back up.
Dexamethasone only works for a short period of time. It doesn't address the underlying cause of my ITP.
Second Line Treatment (Doptelet)
Doptelet is a tablet that stimulates the production of platelets in the bone marrow. My hematologist prescribed 20mg per day while I was in the hospital after my platelet count dropped below 2k. Since then, my platelet count has started to rise and stabilized around 80k.
For the first time in months, I was able to have a normal menstrual cycle—no heavy bleeding, no clots, no fear. I haven’t noticed any side effects from Doptelet. For me, this drug has been life-changing.
But I also know Doptelet is only treating the symptom—low platelet count. It doesn’t address the underlying cause of my ITP. And I’m still determined to find out what triggered it in the first place.
Preparing for Last Resort Treatment (Splenectomy)
My hematologist mentioned that if neither dexamethasone nor Doptelet worked, the final option would be a splenectomy—removal of the spleen. It would be the last resort. I understood that he was being cautious, wanting to prepare for the worst. He suggested I meet with a surgeon to discuss the procedure and begin getting the necessary vaccines.
Both the hematologist and the surgeon assured me the procedure itself is relatively straightforward. In most cases, removing the spleen leads to a rise in platelet count. But they also noted that patients with lupus tend to have less success with splenectomy, and they don’t fully understand why. Splenectomy also carries risks—most notably, a higher susceptibility to infections after the spleen is gone. That’s why my doctor insisted I receive all the required vaccinations beforehand.
Personally, I believe the spleen plays an important role in the immune system. It has a reason to be part of the body, and I don’t want to remove it unless it’s absolutely necessary. It is the last resort that I don't want to take.
Lupus Diagnosis
My hematologist ordered a panel of autoimmune marker tests, and the results came back positive for lupus. He referred me to a rheumatologist, suspecting that lupus might be the underlying cause of my ITP. I was stunned—one autoimmune disease felt like more than enough. Now I was facing the possibility of a second.
At the rheumatologist’s office, more blood work confirmed that I did, in fact, have a mild case of lupus. I had been experiencing occasional joint discomfort, but no flares from sunlight, and I’d never had the classic butterfly rash on my face. The rheumatologist prescribed hydroxychloroquine (HCQ), a medication commonly used to manage lupus. Since HCQ takes time to build up and take effect, I started it right away, hoping it might also help stabilize my platelet count.
Carnivore Diet
One weekend in February 2025, I made handmade noodles for two days, and over the next few days, my platelet count dropped to 2k. Sometimes my hands felt numb or tingly after eating. From reading books, I also learned that most autoimmune diseases are triggered by a leaky gut. I realized that food could be a major factor in my autoimmune condition. To control the food factor, I chose an extreme elimination diet — the carnivore diet — instead of trying to figure out which specific foods were triggering my condition.
H Pylori Infection
In one of the ITP Facebook groups I joined, patients shared their experiences, symptoms, and tips for managing medications. I connected with a woman who had been managing her ITP for years. We often chatted about Doptelet—how to take it, what to expect. Once my platelet count became stable on Doptelet, she suggested I look into Helicobacter pylori (H. pylori). She told me that many ITP patients had tested positive for this stomach bacteria.
I was skeptical at first—I had never had any gastrointestinal issues. But I made a mental note to ask for a test at my next GI appointment. Eventually, I took a breath test for H. pylori. And to my surprise, it came back positive.
Now I had another possible path to find the root cause of my ITP.
My GI doctor immediately prescribed Talicia, a combination antibiotic, to eradicate the H. pylori bacteria. I followed the treatment for 14 days. To my surprise—and my hematologist’s—my platelet count dropped to 40k during the course of antibiotics. Concerned, he increased my dose of Doptelet to 40mg per day. But my platelets didn’t bounce back to the 80k level they had maintained before the antibiotics.
He suggested IVIG again to quickly boost my platelets. But I refused. I wanted to wait and see what my body would do once the antibiotics were out of my system.
Then something unexpected happened: three days after I finished the antibiotics, my platelet count rose to 50k. A week later, it jumped to 126k. Two weeks later, it climbed to 236k.
Then I asked my hematologist to reduce my Doptelet dosage to 20 mg per day. My platelet count dropped to 96k over two weeks, then rose to 126k — higher than the 80s-level I had before starting the antibiotics, even when I was also on 20 mg of Doptelet. This was a very positive sign that treating H. pylori was helping my platelet count!
Blood Results Over Time
Platelet Counts (10^9/L)
Platelet counts are a measure of the number of platelets in a cubic millimeter of blood. Platelets are small cells that help the blood clot and prevent bleeding.
Normal range: 150 - 450 k
- 12/18/2024: 16 (Family doctor visit)
- 12/20/2024: 14 (Family doctor visit, recheck)
- 12/21/2024: 22 (ER visit)
- 12/27/2024: 78 (after 1st round of Dexamethasone)
- 01/02/2025: 14
- 01/08/2025: 82 (after 2nd round of Dexamethasone)
- 01/17/2025: 42
- 01/20/2025: 33
- 01/27/2025: 32
- 02/03/2025: 13
- 02/10/2025: 48 (after 3rd round of Dexamethasone and IVIG)
- 02/14/2025: 2 (hospitalized)
- 02/15/2025: 22 (on Dexamethasone, IVIG and Doptelet 20mg)
- 02/16/2025: 44 (on Dexamethasone and Doptelet 20mg)
- 02/17/2025: 99 (on Dexamethasone and Doptelet 20mg)
- 02/20/2025: 136 (continue Doptelet 20mg from now on)
- 02/24/2025: 112
- 02/27/2025: 81
- 03/03/2025: 93
- 03/06/2025: 80
- 03/10/2025: 73
- 03/17/2025: 89
- 03/24/2025: 49 (after starting antibiotics for H. pylori)
- 03/27/2025: 77 (increasing Doptelet to 40mg/20mg on alternate days 30mg/day)
- 03/31/2025: 40 (increasing Doptelet to 40mg every day 40mg/day)
- 04/03/2025: 37
- 04/07/2025: 47 (after finishing antibiotics for H. pylori)
- 04/11/2025: 126
- 04/17/2025: 236 (reducing Doptelet to 40mg/20mg on alternate days (25% reduction) 30mg/day)
- 04/24/2025: 214 (reducing Doptelet to 20mg every day (33% reduction) 20mg/day)
- 05/01/2025: 168
- 05/07/2025: 96
- 05/15/2025: 123
- 05/23/2025: 138
- 05/30/2025: 126 (tested at Quest Diagnostics in Bay Area, CA)
- 06/06/2025: 148 (tested at a clinic in Shinjuku, Tokyo)
- 06/13/2025: 208 (stopped HCQ 2 days ago, tested at a clinic in Shinjuku, Tokyo)
- 06/19/2025: 182 (tested at a clinic in Shinjuku, Tokyo)
- 06/29/2025: 132 (tested at a clinic in Shinjuku, Tokyo)
- 07/08/2025: 201 (tested at Australian Clinical Labs in Sydney, Australia)
- 07/15/2025: 270 (tested at Australian Clinical Labs in Sydney, Australia. Reducing Doptelet to 20mg every other day (50% reduction)!! 10mg/day)
- 07/22/2025: 204 (tested at Australian Clinical Labs in Sydney, Australia.)
- 08/06/2025: 107 (1st test since getting back home, Reducing Doptelet to 20mg 3 times every 7 days (14% reduction)!! 8.6mg/day)
- 08/28/2025: 118 (Reducing Doptelet to 20mg 3 times every 8 days (12.5% reduction)!! 7.5mg/day)
- 09/24/2025: 105 (Reducing Doptelet to 20mg 3 times every 9 days (11.1% reduction)!! 6.67mg/day)
- 10/01/2025: 101
- 10/22/2025: 99
- 11/19/2025: 57
- 11/20/2025: 62 (at primary care visit)
- 12/05/2025: 95 (Reducing Doptelet to 40mg every 7 days (15% reduction)!! 5.7mg/day)
- 12/22/2025: 74 (at primary care visit)
- 01/31/2026: no testing (manageable period, Reducing Doptelet to 20mg once every 4 days (12.3% reduction)!! 5mg/day)
(to be continued...)
White Blood Cell Count (WBC)
White blood cells are a type of cell in the body that help fight infection and inflammation. Low WBC (leukopenia) can be associated with autoimmune conditions, certain medications, viral infections, bone marrow suppression, or chronic inflammatory diseases.
Normal range: 3.9 - 11.0 x 10^3/uL
- 07/08/2025: 2.9 (tested at Australian Clinical Labs in Sydney, Australia. Without HCQ)
- 07/15/2025: 3.3 (tested at Australian Clinical Labs in Sydney, Australia.)
- 07/22/2025: 2.4 (tested at Australian Clinical Labs in Sydney, Australia.)
- 10/01/2025: 2.3 (Primary care visit at annual checkup)
- 11/20/2025: 3.9 (Primary care visit)
- 12/22/2025: 2.9 (Primary care visit)
ESR (Erythrocyte Sedimentation Rate, mm/hr)
ESR is a blood test that measures how quickly red blood cells settle at the bottom of a test tube. Elevated ESR is often associated with inflammation and autoimmune conditions.
- 12/21/2024: 34 (ER visit)
- 12/27/2024: 28 (Hematologist visit)
- 04/23/2025: 25 (Rheumatologist visit. On HCQ)
- 07/08/2025: 21 (tested at Australian Clinical Labs in Sydney, Australia. Without HCQ)
- 07/15/2025: 19 (tested at Australian Clinical Labs in Sydney, Australia.)
- 07/22/2025: 19 (tested at Australian Clinical Labs in Sydney, Australia.)
- 10/01/2025: 20 (Primary care visit at annual checkup)
- 11/20/2025: 21 (Primary care visit)
- 12/22/2025: 16 (Primary care visit)
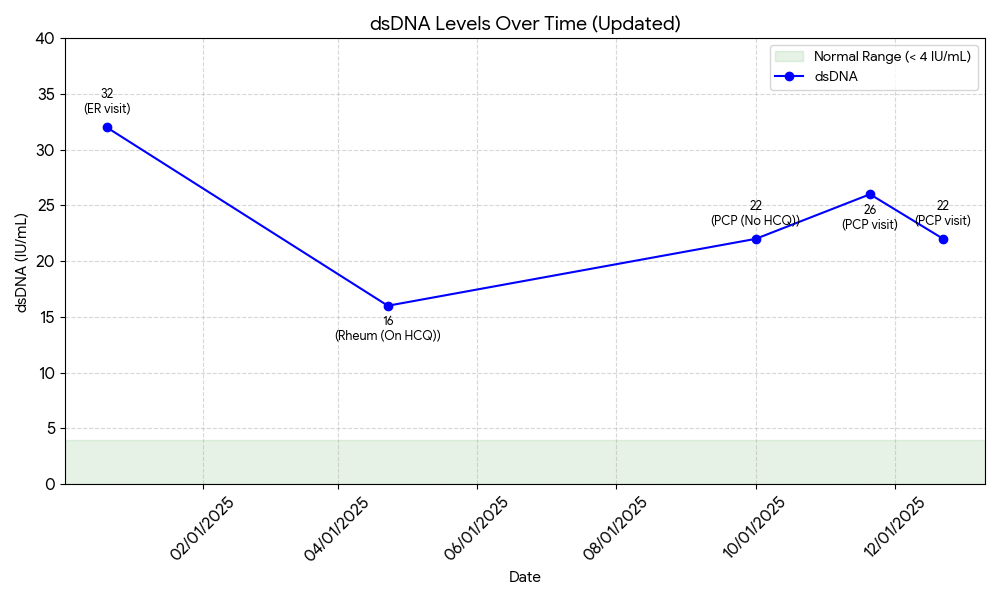
dsDNA (Double-Stranded DNA, IU/mL)
The dsDNA test measures the amount of double-stranded DNA in your blood. Elevated levels of dsDNA are often associated with autoimmune conditions, including lupus.
Normal range: < 4 IU/mL
- 12/21/2024: 32 (ER visit)
- 04/23/2025: 16 (Rheumatologist visit. On HCQ)
- 10/01/2025: 22 (Primary care visit at annual checkup. Without HCQ)
- 11/20/2025: 26 (Primary care visit)
- 12/22/2025: 22 (Primary care visit)
CRP (C-reactive protein, mg/dL)
CRP is a blood test that measures the amount of C-reactive protein in your blood. Elevated levels of CRP are often associated with inflammation and autoimmune conditions.
Normal range: < 0.5 mg/dL
- 04/23/2025: 0.3 (Rheumatologist visit. On HCQ)
- 10/01/2025: <0.3 (Primary care visit at annual checkup. Without HCQ)
- 12/22/2025: <0.3 (Primary care visit)
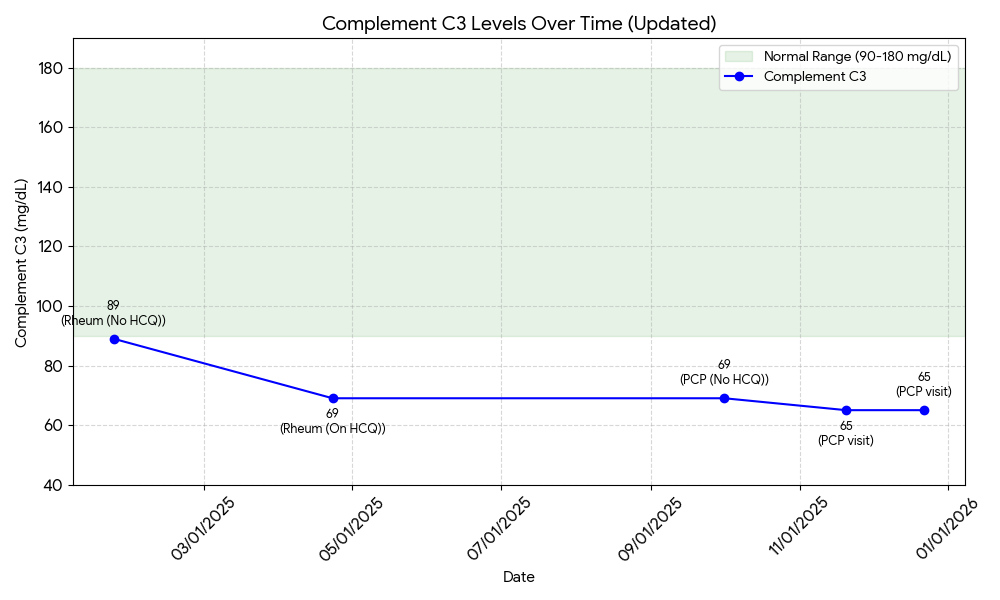
Complement C3 (Complement C3, mg/dL)
Complement C3 is a blood test that measures the amount of complement C3 in your blood. Elevated levels of complement C3 are often associated with autoimmune conditions, including lupus.
Normal range: 90 - 180 mg/dL
- 01/23/2025: 89 (Rheumatologist visit. Without HCQ)
- 04/23/2025: 69 (Rheumatologist visit. On HCQ)
- 10/01/2025: 69 (Primary care visit at annual checkup. Without HCQ)
- 11/20/2025: 65 (Primary care visit)
- 12/22/2025: 65 (Primary care visit)
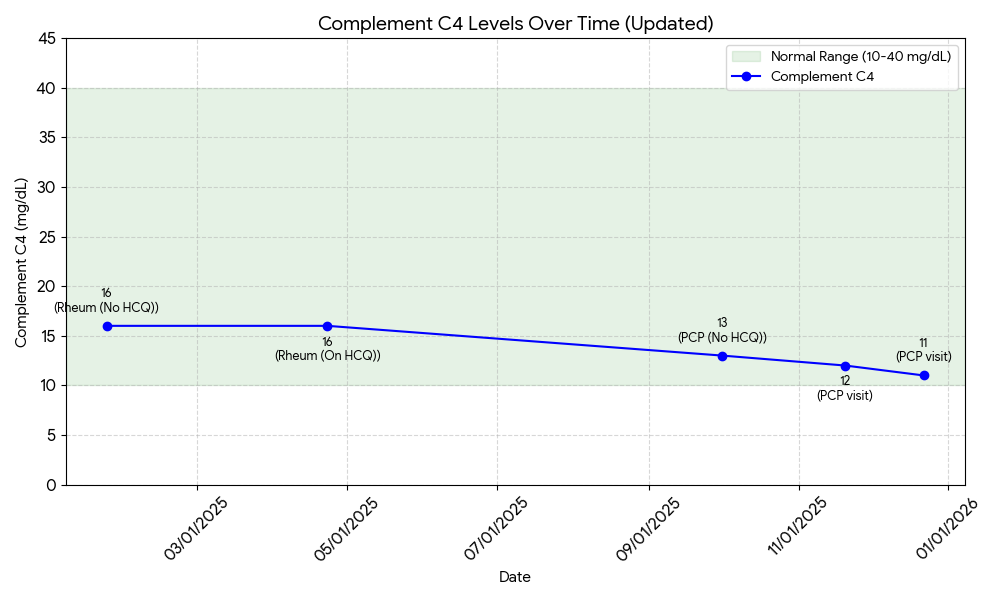
Complement C4 (Complement C4, mg/dL)
Complement C4 is a blood test that measures the amount of complement C4 in your blood. Elevated levels of complement C4 are often associated with autoimmune conditions, including lupus.
Normal range: 10 - 40 mg/dL
- 01/23/2025: 16 (Rheumatologist visit. Without HCQ)
- 04/23/2025: 16 (Rheumatologist visit. On HCQ)
- 10/01/2025: 13 (Primary care visit at annual checkup. Without HCQ)
- 11/20/2025: 12 (Primary care visit)
- 12/22/2025: 11 (Primary care visit)
References
ITP Recovery Example
I came across someone who used natural methods to heal herself without medication. She got rid of H. pylori, and her platelet count gradually increased until she went into remission. She is doing great now and shared a timeline of her platelet count and her treatment.
This gives me an estimate of how long it might take to heal from ITP.
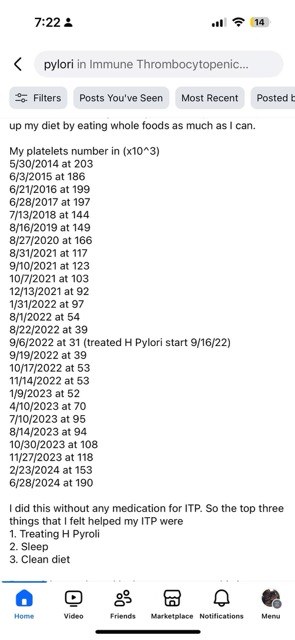
- H pylori treatment to >50k platelets: 2 months
- H pylori treatment to >100k platelets: 12-13 months
- H pylori treatment to >150k platelets: 16 months
- H pylori treatment to ~200k platelets: 20 months




